Research Article
Choosing Repair Technique for Groin Hernias with Patients’ Preferences and Recommendations of Guidelines
Hakan Kulacoglu*
Department of Surgery, Ankara Hernia Center, Ankara, Turkey
*Corresponding author: Hakan Kulacoglu, Department of Surgery, Ankara Hernia Center, Budapeste Caddesi 33/A, Cukurambar, Cankaya, 06530, Ankara, Turkey
Published: 20 Dec, 2017
Cite this article as: Kulacoglu H. Choosing Repair
Technique for Groin Hernias
with Patients’ Preferences and
Recommendations of Guidelines. Clin
Surg. 2017; 2: 1836.
Abstract
Background: Groin hernia is the most frequent type of abdominal wall hernias. Numerous repair
techniques are in use however mesh augmentation is the most frequent. Tailored approach in
inguinal hernia repair is the best way today. Ideally, the choice of repair technique should be a
joint decision of patient and surgeon. In this paper 185 consecutive patients in 2-year period were
analyzed regarding preference for groin hernia repair techniques.
Materials and Methods: All patients are fully informed by the surgeon in the hernia center. Surgeon
explains the characteristics of the patient’s hernia, and tells best possible choices for this hernia
according to the guidelines. Patients’ preference is always of importance, it may not be appropriate
for the hernia or the patient’s medical condition in some cases. Repair technique is eventually
chosen a result of a mutual evaluation. In this study, patients operated by a part-time worker single
surgeon between fall 2015 and fall 2017 were evaluated.
Results: One hundred and eighty-five patients were included (176 male and 9 female). Average age
was 28 (19-85). One hundred and forty patients were treated with open approach (%75); Tissuesuture
repair was performed in three of them. Forty-five patients underwent endoscopic repair.
Thirty-nine patients underwent simultaneous bilateral hernia repairs. Endoscopic repair rate
in bilateral groin hernias was 72%. Five male patients who admitted with a unilateral hernia and
were diagnosed with a concomitant contra-lateral hernia in physical examination did not accept
simultaneous LE repair and underwent unilateral open repair. The reason was high cost of LE
repairs in 3 cases and fear of general anesthesia in two. One female patient with bilateral femoral
hernia did not prefer LE repair because of cost. Ninety-five per cent of the patients were managed in
concordance with guidelines and evidence based medicine.
Conclusion: Tailored approach for the treatment of groin hernias is possible in the vast majority
of the cases. It seems easy and useful to present treatment options to the patients and make a joint
decision together.
Keywords: Hernia; Groin hernia, Inguinal hernia, Femoral hernia; Hernia repair; Mesh;
Guideline; Endoscopic repair; Open repair
Abreviations
LE: Laparoscopic/Endoscopic; TS: Tissure-Suture; TEP: Totally Extraperitoneal
Introduction
Groin hernia is the most frequent type of abdominal wall hernias. Most of groin hernias are iindirect and direct inguinal hernias, whereas femoral hernias are uncommon. Today different repair techniques are in use for groin hernia repairs, however mesh augmentation is most frequently performed procedure. Prosthetic mesh can be placed by either open or Laparoscopic/Endoscopic (LE) approaches. A recent multicenter study revealed that mesh repairs are used in 95% of inguinal hernia repairs [1]. Tissue-Suture repairs (TS) have been used by surgeons with a decreasing rate in last two decades. Cochrane database revealed that Should ice-Bassini suture repair is the best nonmesh technique, however the use of prosthetic augmentation provides lower recurrence rate [2,3]. LE repairs have shown to achieve better outcomes regarding early postoperative pain and return to daily physical activities. These positive effects are more prominent in simultaneous bilateral repairs [3,4]. Tailored approach in inguinal hernia repair is the best way today [5]. Ideally, the choice of repair technique should be a joint decision of patient and surgeon. Surgeon should provide the patient with every information about pros and cons of the repair techniques, and tell them about the guidelines for this particular field. However, many patients admit the hospital with a previous decision about his/her surgery in the era of communication. Some of them may strongly want LE repair, whereas some prefer local anesthesia due to the fear of general anesthesia. In this paper 185 consecutive patients in 2-year period were analyzed regarding preference for groin hernia repair techniques.
Materials and Methods
Ankara Hernia Center is a day surgery center dedicated to treatment of patients with abdominal wall hernias. The center follows evidence based surgery principles. Open repairs of inguinal, femoral, umbilical and epigastric hernias are done in the center at outpatient basis. All laparoscopic-endoscopic hernia repairs, and open repairs of incisional hernias are performed in an affiliated general hospital. When a patient prefers inpatient treatment despite his/her inguinal or umbilical hernia is suitable for day surgery, operation is carried out in the affiliated hospital as well. Patients with severe and complicated systemic diseases are also treated in the hospital. All patients with hernia are fully informed by a single surgeon who specifically works in the field of hernia. Surgeon explains the characteristics of the patient’s hernia, and tells best possible choices for this hernia according to the guidelines. Patients’ preference is always of importance, it may not be appropriate for the hernia or the patient’s medical condition in some cases. Social issues and treatment costs sometimes effects the choice of patients. Repair technique is eventually chosen a result of a mutual evaluation. In this study, patients operated by a part-time worker single surgeon between fall 2015 and fall 2017 were evaluated. Data was recorded prospectively and analyzed afterwards. Patients with primary or recurrent inguinal and femoral hernias are included. Emergency repairs are excluded. The results of this tailored surgery policy are analyzed. Open repairs were performed with three different technique by using local infiltration anesthesia and intravenous sedation [6]. Only mesh procedure is based on Lichtenstein repair [7]. Preperitoneal patch was used in some cases with recurrent hernia following previous open repairs [8]. All LE repairs were performed with Totally Extra peritoneal (TEP) technique under general anesthesia [9,10]. All patients who admitted with unilateral hernia and choose LE repair were recommended to evaluate with ultrasonography to reveal whether a contra lateral hernia exists.
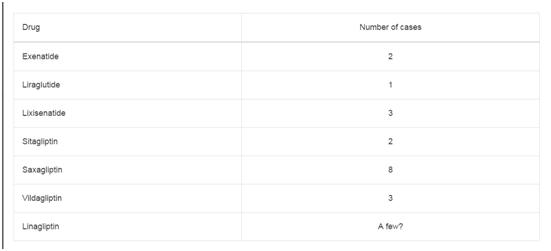
Table 1
Table 2
Results
One hundred and eighty-five patients were operated on during the study period. Four patients who had presented with incarcerated inguinal hernias and had been operated on emergency settings were excluded of the analysis. There were 176 male and 9 female patients. Average age was 28 (19-85). One hundred and forty patients were treated with open approach (%75), TS repair was performed in three of them. Forty-five patients underwent TEP repair (Table 1). No conversion to transabdominal approach or open repair was required. Thirty-nine patients underwent simultaneous bilateral hernia repairs (Table 2). LE repair rate in bilateral groin hernias was 72%. Five male patients who admitted with a unilateral hernia and were diagnosed with a concomitant contralateral hernia in physical examination did not accept simultaneous LE repair and underwent unilateral open repair. The reason was high cost of LE repairs in 3 cases and fear of general anesthesia in two. Three other male patients who admitted with a unilateral hernia and were diagnosed with a concomitant contra lateral hernia with ultrasound chose bilateral TEP. On the other hand, one female patient with bilateral femoral hernia did not prefer LE repair because of cost. Mini mesh repair was performed in this case [11]. Athletes generally chose LE repairs even if they had unilateral hernia. One basketball player underwent simultaneous open mesh repair for bilateral inguinal hernia because of lower cost. Suture repair was chosen by three patients with inguinal hernias (1.6% of whole series). Two male patients did not want prosthetic material and preferred suture repair. One female patient had a small indirect inguinal hernia and a suture repair was a mutual decision. Overall, 9 of 185 patients could not be treated according to the guidelines. In other word, 95% of the patients in a two-year period were managed in concordance with guidelines and evidence based medicine. Patient satisfaction is excellent in all patients but two bilateral repair cases. One male patient with bilateral inguinal hernias and one female patient with bilateral femoral hernias, both underwent open repairs, were not happy with their early postoperative comfort. No foreign body sensation was recorded in follow-up.
Discussion
Inguinal hernia repair is one of the most common procedures in general surgery. Numerous repair techniques have been described, among them mesh repairs are widely used today because of their low recurrence rates [12]. Although Should ice Hospital achieves a very low cumulative recurrence rate by performing its own four-layer tissue suture technique which is very similar to original triple-layer Basssini repair described in 1890 [13-15]. The number of institutions that specifically dedicated to treatment of abdominal wall hernias has been increasing [16]. A specific hernia center should have the tasks of dissemination of up-to-date knowledge, and scientific publications of work for its patients and colleagues. It is crucial to follow current guidelines and evidence based medicine. Although there is a wide spectrum for technical preference there is an also clear algorithm for specific type of cases. For example, many elderly patients are not suitable for general anesthesia because of systemic diseases and generally managed by open repiars with local anesthesia [17]; patients with bilateral hernias are very good candidates for LE repairs [4,18,19]; female patients are also considered for LE approach to observe a possible femoral hernia during the procedure [Guidelines x 2]. Today, many patients with groin hernias admit to hospitals with an opinion about technical approach for repair. Internet searches and related websites are very useful for the patients, whereas patient-topatient recommendations and personal experience transfer is quite common. No doubt, the surgical skill and experience of the surgeon and resources of the institution are important factors. A hernia specific surgeon should be capable of performing all kind of repairs and prefers the one which is most suitable for the case. Des Côteaux and Sutherland conducted a survey by mailed questionnaire for the fellows of the Royal College of Physicians and Surgeons of Canada in 1999 [20]. The preferred techniques for repair of primary inguinal hernias were 15% for LE repair and 85% for open techniques. Open techniques were lined up as Bassini, mesh plug, Lichtenstein, Should ice and McVay. In a recent web-based survey among general surgeons in North America 46% of respondents never perform LE repairs [21]. Surgeons preferred LE approach for bilateral and recurrent inguinal hernias with rates of 48% and 44% respectively. A similar survey was conducted during the 18th Congress of the European Association of Endoscopic Surgeons [22]. Eighty two percent of surgeons preferred a tailored approach, whereas 18% always used the same technique. LE approaches are used more frequently than the open repair in bilateral (7 vs. 93%) and recurrent hernias (19 vs. 81%), whereas open repair was used in one third. Another type of survey was carried out by asking the physicians and surgeons "If you had an inguinal hernia, how would you prefer to have it repaired?”In 1992, when laparoscopic repairs were just being introduced, Atabek et al. [23] in USA conducted a survey to determine current experience and preference levels of general surgeons for laparoscopic hernia repair [23]. Only 8% of the respondents preferred laparoscopic repair for their imaginary unilateral inguinal hernia. A similar survey was performed in 1999 among surgeons in Ankara, Turkey [24]. Only 14.1% of the respondents preferred a laparoscopic hernia repair. Personal laparoscopic herniorrhaphy experience significantly affected the choice. Among respondents who had performed no laparoscopic hernia repair, only 10.2% preferred laparoscopic technique for their own inguinal hernias, whereas the preference rate rose to 33.3% in other who had previously done laparoscopic hernia repair. This survey was repeated ten years later. In general, 88.9% of the respondents preferred open repair, while only 11.1% chose laparoscopy [25]. In all three surveys the majority of the participants who preferred an open repair stated that it was a better-known technique to prefer. Almost half considered local anesthesia an advantage. Laparoscopic repair was mainly preferred for its advantages of less pain and early return to work. Nevertheless, it was recently reported that laparoscopic repair rate for groin hernias increased between 2005 and 2010. LE repair rates for groin hernias show differences between countries. In the year 2001-02, 95.9% of mesh repairs were performed by open surgery, and 4.1% of repairs were performed by LE surgery in England [26]. However, higher rates existed in some European countries, North America and Far East. The classical considerations for LE repairs are the availability of equipment, familiarity with the anatomy when using these techniques, operative time, cost to the patient, and the potential need to convert to an open procedure [27]. However, as Sharma and Chelawat reported, the world is in an era of witnessing a shift away from surgeon-defined conditions to patient-defined benefits. Patients become more aware of the options for hernia repair and share their experiences with others. This render more patients are likely to demand a specific repair approach. As this situation is merged with increasing experience of the surgeons, the rate of LE repairs is rising. In the present study, 75% of the groin hernia patients were treated with open approach. This rate became reversed for bilateral hernias as recommended by the guidelines. However, LE could not be performed in some cases of bilateral hernia because of high cost. Some patient rejected simultaneous bilateral repair because the lack of complaint at contra lateral side. TS repairs may provide good outcomes in properly selected cases. Low recurrence rates can be achieved with Should-Bassini technique, however complete anatomy knowledge and surgical experience is the key. In this series, a very small part of patient population was treated with TS repair. Patient’s fear of prosthetic material should be understood and accepted by surgeons, because some patients admit after reading scientific publications and informative pages about mesh complications in the internet [28-30]. Advantages and disadvantages of TS repair and mesh augmentation should be explained and the patient should make his/her own decision freely. In conclusion, tailored approach for the treatment of groin hernias is possible in the vast majority of the cases. It seems easy and useful to present treatment options to the patients and make a joint decision together. High patient satisfaction is possible with evidence based approach and working in accordance to guidelines.
References
- Seker G, Kulacoglu H, Öztuna D, Topgül K, Akyol C, Çakmak A, et al. Changes in the frequencies of abdominal wall hernias and the preferences for their repair: a multicenter national study from Turkey. Int Surg. 2014;99(5):534-42.
- Scott NW, McCormack K, Graham P, Go PM, Ross SJ, Grant AM. Open mesh versus non-mesh for repair of femoral and inguinal hernia. Cochrane Database Syst Rev. 2002;(4):CD002197.
- Köckerling F, Schug-Pass C. Tailored approach in inguinal hernia repair - decision tree based on the guidelines. Front Surg. 2014;1:20.
- McCormack K, Scott NW, Go PM, Ross S, Grant AM. EU Hernia TrialistsCollaboration. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev. 2003;(1):CD001785.
- Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13(4):343-403.
- Köckerling F, Schug-Pass C. Tailored approach in inguinal hernia repair - decision tree based on the guidelines. Front Surg. 2014;1:20.
- Kulacoglu H, Ozyaylali I, Yazicioglu D. Factors determining the doses of local anesthetic agents in unilateral inguinal hernia repair. Hernia. 2009;13(5):511-6.
- Amid PK. Lichtenstein tension-free hernioplasty: its inception, evolution, and principles. Hernia. 2004;8(1):1-7.
- Nyhus LM. The recurrent groin hernia: therapeutic solutions. World J Surg. 1989;13(5):541-4.
- Ferzli GS, Massad A, Albert P. Extraperitoneal endoscopic inguinal hernia repair. J Laparoendosc Surg. 1992;2(6):281-6.
- McKernan JB, Laws HL. Laparoscopic repair of inguinal hernias using a totally extraperitoneal prosthetic approach. Surg Endosc. 1993;7(1):26-8.
- Kulacoglu H. Mini-mesh repair for femoral hernia. Int J Surg Case Rep. 2014;5(9):574-6.
- Kulacoglu H. Current options in inguinal hernia repair in adult patients. Hippokratia. 2011;15(3):223-31.
- Castrini G, Pappalardo G, Trentino P, Correnti FS. The original Bassini technique in the surgical treatment of inguinal hernia. Int Surg. 1986;71(3):141-3.
- Read RC. The centenary of Bassini's contribution to inguinal herniorrhaphy. Am J Surg. 1987;153(3):324-6.
- Shouldice EB. The Shouldice repair for groin hernias. Surg Clin North Am. 2003;83(5):1163-87.
- Kulacoglu H, Oztuna D. Current Status of Hernia Centres around the Globe. Indian J Surg. 2015;77(3):1023-6.
- Kulacoglu H, Alptekin A. Current options in local anesthesia for groin hernia repairs. Acta Chir Iugosl. 2011;58(3):25-35.
- Miserez M, Peeters E, Aufenacker T, Bouillot JL, Campanelli G, Conze J, et al. Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2014;18(2):151-63.
- David L Sanders, Martin Kurzer. British Hernia Society Groin Hernia Guidelines. Issues in Professional Practice (IIPP). Association of Surgeons of Great Britain and Ireland. London, UK. 2013.
- DesCôteaux JG, Sutherland F. Inguinal hernia repair: a survey of Canadian practice patterns. Can J Surg. 1999;42(2):127-32.
- Trevisonno M, Kaneva P, Watanabe Y, Fried GM, Feldman LS, Lebedeva E, et al. A survey of general surgeons regarding laparoscopic inguinal hernia repair: practice patterns, barriers, and educational needs. Hernia. 2015;19(5):719-24.
- Morales-Conde S, Socas M, Fingerhut A. Endoscopic surgeons' preferences for inguinal hernia repair: TEP, TAPP, or OPEN. Surg Endosc. 2012;26(9):2639-43.
- Atabek U, Spence RK, Pello M, Alexander J, Story L, Camishion RC. A survey of preferred approach to inguinal hernia repair: laparoscopic or inguinal incision? Am Surg. 1994;60(4):255-8.
- Kulaçoglu HI, Ozmen MM, Oruç MT, Koç M, Kama NA. Laparoscopic herniorrhaphy: preference rate among surgeons in Ankara, Turkey. East Afr Med J. 2001;78(4):216-9.
- Genc V, Ensari C, Kulacoglu H, Ersoy E, Ergul Z. A questionnaire study on the surgeons' preferences for inguinal hernia repair after a decade. J Coll Physicians Surg Pak. 2009;19(11):744-6.
- National Institute for Health and Care Excellence. Laparoscopic surgery for inguinal hernia repair. Technology appraisal guidance [TA83] 2001 London: National Institute for Clinical Excellence.
- Sharma A, Chelawat P. Endo-laparoscopic inguinal hernia repair: What is its role? Asian J Endosc Surg. 2017;10(2):111-8.
- Seker D, Kulacoglu H. Long-term complications of mesh repairs for abdominal-wall hernias. J Long Term Eff Med Implants. 2011;21(3):205-18.
- Iakovlev VV, Guelcher SA, Bendavid R. Degradation of polypropylene in vivo: Amicroscopic analysis of meshes explanted from patients. J Biomed Mater Res B ApplBiomater. 2017;105(2):237-48.