Case Report
Survey on Patients’ Awareness of the Single Port Laparoscopy for Cholecystectomy
Stephen Chang Kin Yong* and Jeremy Lee Kay Hock
Department of Surgery, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
*Corresponding author: Stephen Chang Kin Yong, Department of Surgery, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Published: 18 Dec, 2017
Cite this article as: Yong SCK, Hock JLK. Survey on
Patients’ Awareness of the Single Port
Laparoscopy for Cholecystectomy. Clin
Surg. 2017; 2: 1828.
Abstract
Introduction: Single-incision Laparoscopic Cholecystectomy (SILC) is a relatively new procedure in
the management of gall bladder disease, compared to Conventional Laparoscopic Cholecystectomy
(CLC). We aim to assess the awareness of SILC and its benefits, amongst patients who had undergone
cholecystectomy.
Materials and Methods: We surveyed 54 patients who had undergone cholecystectomy through
phone interviews (SILC=44/CLC=10).
Results: 70% of the patients surveyed were unaware of SILC prior to their operation. Of the
remaining patients who were aware of SILC prior to their operation, 24% attained SILC information
by word of mouth, 4% from online sources and 2% from newspapers 83% of the patients believe that
SILC is a less painful procedure as compared to CLC. 98% of the patients think that SILC is more
beneficial cosmetically 50% of the patients expect that SILC would cost at least $4000 more than
CLC 44% of the patients thought that SILC has been present in Singapore for at least 1-3 years. 100%
of the patients would recommend SILC to other patients.
Conclusion: The majority of surveyed patients were unaware of SILC prior to their operation.
However, they believed that SILC is more beneficial cosmetically and with reduced post-operative
pain as compared to CLC. All of them would recommend SILC to other patients.
Keywords: Single-incision laparoscopic cholecystectomy; Conventional laparoscopic
cholecystectomy; Gall bladder; Awareness of patients
Introduction
Laparoscopic cholecystectomy was traditionally performed using multiple tiny incisions. SILC was introduced as an alternative procedure to improve cosmesis and reduce post-operative pain [1- 2]. SILC is performed via a single-entry point at the patient’s umbilicus, hence leaving behind a small and barely perceptible scar after surgery [3]. SILC also presents other benefits like reduced hospital stays [4]. In this study we assessed the knowledge of SILC amongst patients who had undergone cholecystectomy and determined whether they would recommend this procedure over the CLC.
Materials and Methods
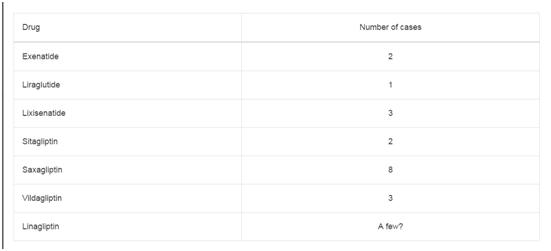
We conducted phone surveys, in English or Mandarin, of all patients who underwent cholecystectomy by a single surgeon from May 2016 to June 2017. The 7 survey questions as shown in (Figure 1) were to assess the patients’ awareness of SILC (4 questions), benefits (2 questions) and if they would recommend this procedure to other patients (1 question). All the data collected is shown in (Table 1). Basic demographic data of the participants collated includes age, gender and ethnicities. Participants completed the survey either independently or with the aid of a translator. The comparison in responses between SILC and CLC patients is shown in (Table 2 and 3). The Chi square statistical test and Fisher’s exact test were used to analyse the difference in responses between SILC and CLC patients. There is deemed to be statistical significance in the data if P <0.050.
Results
We surveyed 54 patients who had undergone SILC or CLC by a single surgeon from May 2016 to June 2017. There were 28 male and 26 female patients. The ages of the patients are between 31 years and 79 years. There were 47 Chinese, 5 Indians and 2 of other ethnicities. During our phone interviews, 6 patients could not speak English or Mandarin (11%), and required a translator. The remainder 48 patients (89%) completed the survey without any assistance. Table shows the responses to the survey about SILC for the patients who had undergone cholecystectomy (Table 1). Patients were first asked if they were aware of SILC prior to their operation. 70% of the patients were unaware of SILC prior to their operation, whilst 30% were aware. The 30% who were aware of SILC were then asked how they received the SILC information 24% had attained the SILC information by word of mouth from their relatives, 4% from online sources, 2% from newspapers and 0% from medical journals and articles. All of the patients were asked if they believed that SILC will have reduced post-operative pain as compared to CLC. 83% believed that SILC will have reduced post-operative pain, whilst 17% did not believe so. Patients were then asked if they thought that SILC is more beneficial cosmetically as compared to CLC. 98% of the patients thought that SILC is more beneficial cosmetically, whilst 2% did not think so. Patients were then asked how much more they think the SILC procedure would cost as compared to CLC. 15% of the patients indicated $2000 to $3000, 35% indicated $3000 to $4000, and 50% indicated more than $4000. Patients were then asked how long they think SILC has been performed in Singapore. 44% indicated 1 to 3 years, 28% indicated 4 to 6 years, and 28% indicated more than 6 years. In our last question, patients were asked if they would recommend SILC to other patients. 100% of the patients said that they would do so. The differences in responses between the SILC and CLC patients are shown in (Table 2 and 3). It was determined that there was no significant statistical difference between SILC and CLC patients on their awareness of SILC prior to their operation, i.e. P=0.512. However, there was significant statistical difference in the responses when 90% of SILC patients compared to 50% of CLC patients believed that SILC will have reduced post-operative pain, i.e. P=0.002. It was determined that there was no significant statistical difference in the responses from SILC and CLC patients on whether they thought SILC is more beneficial cosmetically, i.e. P=0.185. There was also no significant statistical difference in the patients’ responses on whether they would recommend SILC to other patients, i.e. P=1.000.
Figure 1
Table 1
Table 2
Table 3
Discussion
Single Incision Laparoscopic Cholecystectomy was first performed in 1997 by Navarra, using two trocars through one sub umbilical incision and three abdominal stay sutures to aid in gallbladder retraction [5]. This paper is the first study to assess the awareness of SILC amongst patients who had undergone cholecystectomy. Our main finding was that most patients (70%) were unaware of SILC prior to their operation. This is surprisingly so as SILC has been performed for almost 10 years now in Singapore and there are an increasing number of surgeons who can offer SILC for cholecystectomy. Amongst the remaining patients (30%) who were aware of SILC prior to their operation, a majority of patients had attained SILC information by word of mouth (24%) and only a small number of patients attained their information from online sources (4%) and newspapers (2%). This is partly because there have been limited coverage of this technique by the mainstream media such as the newspaper. However, given that the Singapore population has easy access to online sources, the finding of only 4% of the study population who knew about such a procedure from online sources was quite surprising. None of the patients had received SILC information from medical journals and articles. This is not surprising as in our current healthcare practice; patients are still very much reliant on doctors for medical information instead of performing their own research in medical journals. Most of the SILC information had been disseminated by word of mouth through relatives who had previously undergone SILC procedures. This exemplifies the good outcomes that SILC can provide. SILC being a leading technology would require specialised skill set and additional equipment. Studies have shown that with this additional skill set and equipment, SILC can bring about increased benefits such as reduced post-operative pain and better cosmesis [6]. With such benefits, a majority of patients (50%) would expect the cost of SILC to be at least $4000 more than CLC. We had done a comparison in responses between SILC and CLC patients. The survey shows that 50% of CLC patients thought that SILC will have reduced post-operative pain, and 90% believed that SILC is more beneficial cosmetically. Among the CLC patients who were aware of SILC prior to their operation, all had opted to go for CLC. This is likely due to the lower operations costs. However, it is interesting to note that all the patients who underwent CLC would recommend SILC to other patients. Further improvements can be made for future studies. Firstly, the use of a translator can bridge communication gaps between patients and interviewers. Secondly, visual aids (Presentation slides, models or pictures) could be used to explain the merits of SILC over CLC.
Conclusion
This study confirms that despite relatively low awareness of SILC amongst the patients, the general consensus is that SILC is likely to be more beneficial cosmetically and will reduce post-operative pain, and that they will all recommend SILC to other patients. In Singapore, SILC is still not a mainstream surgical option due to the low level of awareness. Doctors should introduce the SILC option while counselling the patients for cholecystectomy. This will provide patients with additional information to make a better informed decision of their surgical option for cholecystectomy.
References
- Borle FR, Mehra B, Singh AR. Comparison of Cosmetic Outcome between Single-Incision Laparoscopic Cholecystectomy and Conventional Laparoscopic Cholecystectomy in Rural Indian Population: A Randomized Clinical Trial. Indian J Surg. 2015;77(3):877-80.
- Chang SK, Wang YL, Shen L, Iyer SG, Madhavan K. A randomized controlled trial comparing post-operative pain in single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy. World J Surg. 2015;39(4):897-904.
- Li T, Kim G, Chang S. Tips and tricks to avoid bile duct injury in SILC: an experience of 500 cases. Surg Endosc. 2016;30(11):4750-5.
- Joseph S, Moore BT, Sorensen GB, Earley JW, Tang F, Jones P, et al. Single-incision laparoscopic cholecystectomy: a comparison with the gold standard. Surg Endosc. 2011;25(9):3008-15.
- Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. - Br J Surg. 1997;84(5):695.
- Chang SK, Lee KY. Therapeutic advances: Single incision laparoscopic hepatopancreatobiliary surgery. World J Gastroenterol. 2014;20(39):14329-37.