Research Article
Pilot Telephone Intervention to Improve Survivorship Care in Patients with Head and Neck Cancer
Thanh P Ho1, Mary Jewison2, Kathryn J Ruddy2 and Katharine AR Price2*
1Department of Internal Medicine, Mayo Clinic, Rochester, Minnesota, USA
2Department of Medical Oncology, Mayo Clinic, Rochester, Minnesota, USA
*Corresponding author: Katharine AR Price, Department of Medical Oncology, Mayo Clinic, 200 First Street SW, Rochester, MN, 55905, USA
Published: 01 Dec, 2017
Cite this article as: Ho TP, Jewison M, Ruddy KJ, Price
KAR. Pilot Telephone Intervention to
Improve Survivorship Care in Patients
with Head and Neck Cancer. Clin Surg.
2017; 2: 1795.
Abstract
Background: Multimodality treatment for Head and Neck Cancer (HNC) is associated with
significant impact on quality of life and underscores the importance of comprehensive survivorship
care.
Objective: A pilot phone intervention was conducted in HNC survivors to improve coordination of
care by addressing core problems: dysphagia, lymphedema, neck pain, fatigue, emotional distress,
financial concerns, and nicotine dependency.
Methods: Patients who had completed curative intent therapy for HNC were identified. One month
prior to an upcoming appointment, patients were called by a nurse who asked about common longterm
side effects and offered services and additional appointments as indicated.
Results: Forty-eight patients (38 males, 79%) with a median age of 60 years (range 41 to 78)
were contacted. Most were stage IVA HNC (34 patients, 92%), squamous cell carcinoma (44,
92%) and located in the oropharynx (28, 58%). Patients were contacted between 6 to 77 months
from definitive therapy, with conversations ranging from 3 to 30 minutes. Common symptoms
included neck pain (52%), dysphagia (46%), and lymphedema (19%). Fatigue (33%) and emotional/
psychological concerns (27%) were also noted. Financial matters (10%) and smoking cessation (4%)
were infrequently reported. Ultimately, 31% of conversations led to referrals or other interventions
resulting in a change in management.
Limitations: The sample size was small, and no direct patient outcomes were reported.
Conclusion: This study demonstrates the need for comprehensive and coordinated survivorship
care for patients with HNC.
Keywords:Head and neck cancer; Survivorship; Dysphagia; Lymphedema; Fatigue; HPV;
Oropharynx
Abbreviations
HNC: Head and Neck Cancer; HPV: Human Papillomavirus; HPV-OPC: HPV-Positive Oropharynx Cancer; IRB: Institutional Review Board; OS: Overall Survival
Introduction
Historically, Head And Neck Cancer (HNC) was associated primarily with tobacco and alcohol
use, with 40% to 60% Overall Survival (OS) rates for most patients with locally-advanced disease
[1-3]. However, in recent decades, the incidence of Human Papillomavirus (HPV)-associated
oropharyngeal cancer has been steadily increasing; in men in the United States, this is now the
eighth most common cancer [4]. The prognosis of HPV-Positive Oropharynx Cancer (HPV-OPC)
is significantly better, with three year OS in never-smokers approximately 90% [5]. In addition,
patients with HPV-OPC are typically younger, healthier, and have less history of tobacco use than
patients with HPV-negative HNC. As a consequence, patients with HNC are being cured at higher
rates and most will be expected to live decades with treatment-related side effects. Treatment for
locally-advanced HNC typically involves a combination of surgery, radiation, and chemotherapy.
This multimodality therapy is associated with long-term treatment-related side effects such as
xerostomia, dysphagia, pain, lymphedema and fatigue.
Improved survival rates for many patients with HNC combined with substantial treatment morbidities create a need for comprehensive survivorship care for this patient population. In elderly patients with laryngeal squamous cell
cancer, higher quality care has been associated with both improved
survival and reduced cost [6]. One challenge in clinical practice is
to identify and offer referrals to manage long-term side effects in
an efficient and coordinated fashion. In October 2013, Mayo Clinic
in Rochester, Minnesota began an HNC survivorship initiative to
better address the needs of these patients. A multi-disciplinary team
of clinicians compiled an extensive list of survivorship issues with
potential interventions. Of the 52 clinician-identified survivorship
issues, seven were chosen to be addressed in a clinical phone pilot
based on the fact that 1) They are common problems in clinical
practice and 2) established clinical interventions or referrals exist
to address these issues. Theses even survivorship issues included:
dysphagia, lymphedema, neck pain, fatigue, financial concerns,
emotional distress, and nicotine dependency.
At this comprehensive cancer center, standard follow-up care
after completion of treatment for HNC includes multidisciplinary
follow-up with otolaryngology-head and neck surgery, radiation
oncology, and medical oncology visits every three months for the first
two years after treatment, then every six months for three years, and
then annually after five years. These appointments offer point-of-care
opportunities to intervene on long-term side effects of treatment. In
the current practice, many patients travel from distant locations for
follow-up care, and it can be challenging to get appointments at short
notice when an active issue is identified during the clinic follow-up
visit. In February 2014, a phone pilot was initiated to proactively
identify symptoms prior to a patient’s appointment, with the focus
ondysphagia, lymphedema, neck pain, fatigue, financial concerns,
emotional distress, and nicotine dependency. The goal of the phone
pilot was to improve coordinated survivorship care. This manuscript
reports the results of this clinical phone pilot.
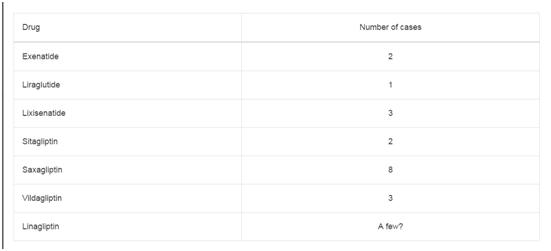
Table 1
Methods
The phone pilot was conducted by a dedicated HNC nurse in the Division of Medical Oncology at Mayo Clinic in Rochester, Minnesota. Patients were identified for the pilot based on the following criteria 1) Had completed definitive (curative-intent) therapy for a HNC and 2) Had a follow-up appointment scheduled in medical oncology within one month after the pilot phone call. During the phone call, the nurse inquired about the patient’s overall health status and asked specifically about the seven above-specified target areas. A data collection sheet was completed at the time of the phone call that documented patient responses to the target questions and whether the phone call resulted in any additional appointments, referrals, or other actions. Additional data such as cancer stage and therapy were abstracted from the electronic medical record using retrospective chart review. The study was approved by the institution’s Institutional Review Board (IRB). Descriptive studies were performed using JMP® (Carey, North Carolina).
Results
Demographics: Forty-eight patients (38 males, 79%) were
contacted; the majority were white (47 patients, 98%; Table 1). Over
half (27 patients, 56%) did not have a significant smoking history. The
median age at diagnosis was 60 years (range 41 to 78). The median
time since definitive treatment was 21 months (range 6 to 77 months).
Cancer characteristics: The majority of patients were stage IVAHNC (34 patients, 92%; Table 1), predominantly squamous
cell carcinoma (44 patients, 92%) and located in the oropharynx
(28 patients, 58%). Human Papillomavirus (HPV) positivity, per
pathologic staining for antibodies to p16 or HPV in-situ hybridization
studies, was reported for 19 patients (68%) with oropharyngeal
squamous cell carcinoma. Most patients received surgery (62%),
radiation (98%), and systemic therapies (96%).
Pilot intervention: Phone conversations lasted 10.37 ± 7.13
minutes on average (median 7 with range from 3 to 30 minutes).
Thirty-seven individuals (77%) expressed concern about at least one
topic (Table 2). This led to 15 referrals or other interventions (31% of
conversations) with 10 messages sent to providers in other disciplines
(21%) and 8 changes in upcoming appointments (17%).
Neck pain or stiffness was reported by over half of patients (25
patients, 52%); six of them received interventions including referrals
to cancer rehabilitation or physical medicine and rehabilitation, or
resources on acupuncture. Two who did not receive interventions
had previously tried acupuncture or massage therapy without
significant benefit. Lymphedema was a concern for 9 patients
(19%), although many also reported that their lymphedema was
improving. Concern over lymphedema resulted in 1 intervention
(2%), a referral to cancer rehabilitation that included consultation
with a lymphedema therapist. Another patient had previously been
evaluated by a lymphedema specialist. Of the 25 individuals with neck
pain or stiffness, 6 patients also had difficulty with lymphedema.
During these phone conversations, 22 patients (46%) reported
difficulty swallowing, resulting in 4 interventions that included
prescription for Biotene® as well as patient-specific resources on
acupuncture. Two patients already had scheduled endoscopy and
swallow study, respectively, at the time of phone call.
Patients also expressed a range of psychological and emotional
concerns (13 patients, 27%) including anxiety, depression, anger,
cognitive changes related to memory, issues with self-esteem or the
workplace. This resulted in 7 interventions (15%). Support groups,
stress management brochures, and referrals to psychiatry or social
work were offered. Two declined interventions and preferred to
discuss their concerns with their oncologist or primary care physician
instead. Similarly, energy level was a concern for 16 patients (33%),
with 2 (4%) receiving pamphlets on potential solutions tailored to
specific patient interest, such as yoga or tai chi. Six patients (13%)
endorsed both fatigue and psychosocial concerns.
Less commonly, patients reported financial concerns (5 patients,
10%); no interventions were performed. One patient opted, instead,
to discuss these issues during his medical oncology follow up
appointment. Two patients (4%) expressed difficulty with smoking
dependence; one was offered nicotine cessation clinic and the other
was already utilizing nicotine patches to reduce nicotine use.
These phone calls encouraged patients to discuss other medical
concerns as well; for instance, one resulted in physical therapy referral
for shoulder pain (without reporting neck pain). In another instance,
the nurse spoke with the patient’s spouse, who was “extremely happy
to get the call”, and agreed to receive educational materials by mail.
Table 2
Discussion
HNC survivors who undergo multidisciplinary therapy may
experience significant treatment-related side effects that can impact
quality of life. Individuals with late-stage tumors report significantly
worst quality of life scores on areas such as swallowing and social
contact [7]. Long-term overall quality of life can decline, as reported
by a study on 10-year survival [8]. We present a telephone-based pilot
intervention to address common side effects experienced by HNC
survivors. Our study demonstrates that even for patients several years
from definitive treatment, symptoms such as dysphagia and neck pain
often persist. The challenges of assessing and treating dysphagia may
contribute to this [9]. We found that a medical oncology nurse-based
phone call helped to identify patients with specific symptoms (usually
related to radiation or surgery) for which targeted interventions (e.g.,
endoscopy or physical medicine and rehabilitation) could be helpful,
it not already scheduled.
Our pilot intervention also identified and addressed important
psychosocial concerns in HNC survivors. We found that fatigue,
anxiety, and/or depression, present in nearly a third of all participants
and often persist long after completion of treatment. Poor body image
among this cohort can contribute to depressive symptoms [10], and
individuals with HNC, especially those with cancer of the larynx
and hypopharynx, are at increased risk of suicide [11]. It remains
unclear if psychosocial factors contribute to survival, and others
studies have attempted to assess this association or predict survival
based on quality of life scores [12,13]. It is apparent, by our study and
others, that psychological distress is common in this unique patient
population but may be under-recognized or undertreated [14].
This pilot study underscores the importance of coordinated,
multidisciplinary survivorship care. Many of the concerns that were
reported by these HNC survivors are best addressed by non-oncology
specialties including primary care providers, gastroenterologists,
physical medicine and rehabilitation specialists, and psychiatrist/
psychologists. In addition, the effectiveness of this phone pilot
highlights the value of patient contact that is not necessarily a faceto-
face evaluation. Although a telephone-based nursing assessment
does require staff resources, the average length of each phone call was
only ten minutes. It is notable that 31% of the phone calls resulted in
a tangible change to a patient’s upcoming appointment schedule. In
the future, it is possible that text- or web-based communication could
serve a similar purpose.
The primary limitation of this study was its small sample size.
In addition, no direct patient-reported outcomes were collected due
to limited resources. Therefore, we were not able to compare this
telephone-based intervention to standard care with regard to patient
satisfaction and physical and mental quality of life. However, this
hypothesis-generating study did have a wide age range of patients
with HNC, from 41 to 78 years old, suggesting that our findings are
reasonably generalizable across the age spectrum. Due to the size of
the study, sex-specific analysis was not performed. With improving therapies that may prolong life in HNC, survivorship care should
address therapy-related side effects in addition to the impact of
emotional and psychological challenges of cancer treatment. In light
of rising numbers of cancer survivors, the future of survivorship care
will likely involve utilizing resources such as phone interventions
and web-based programs to provide comprehensive, coordinated
survivorship care.
Acknowledgement
The authors thank Julie Schutte, R.N., O.C.N.; Pearl Pham, P.A.-C.; Jessica Brandt, R.N., O.C.N. and Sadie Flatt, R.N. for their assistance with clinical care and coordination of care on this study.
References
- Calais G, Alfonsi M, Bardet E, Sire C, Germain T, Bergerot P, et al. Randomized trial of radiation therapy versus concomitant chemotherapy and radiation therapy for advanced-stage oropharynx carcinoma. J Natl Cancer Inst. 1999;91(24):2081-6.
- Forastiere AA, Goepfert H, Maor M, Pajak TF, Weber R, Morrison W, et al. Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med. 2003;349(22):2091-8.
- Adelstein DJ, Li Y, Adams GL, Wagner H Jr, Kish JA, Ensley JF, et al. An intergroup phase III comparison of standard radiation therapy and two schedules of concurrent chemoradiotherapy in patients with unresectable squamous cell head and neck cancer. J Clin Oncol. 2003;21(1):92-8.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7-30.
- Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tân PF, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363(1):24-35.
- Gourin CG, Starmer HM, Herbert RJ, Frick KD, Forastiere AA, Quon H, et al. Quality of care and short- and long-term outcomes of laryngeal cancer care in the elderly. Laryngoscope. 2015;125(10):2323-9.
- Chaukar DA, Walvekar RR, Das AK, Deshpande MS, Pai PS, Chaturvedi P, et al. Quality of life in head and neck cancer survivors: a cross-sectional survey. Am J Otolaryngol. 2009;30(3):176-80.
- Mehanna HM, Morton RP. Deterioration in quality-of-life of late (10-year) survivors of head and neck cancer. Clin Otolaryngol. 2006;31(3):204-11.
- Schindler A, Denaro N, Russi EG, Pizzorni N, Bossi P, Merlotti A, et al. Dysphagia in head and neck cancer patients treated with radiotherapy and systemic therapies: Literature review and consensus. Crit Rev Oncol Hematol. 2015;96(2):372-84.
- Rhoten BA, Deng J, Dietrich MS, Murphy B, Ridner SH. Body image and depressive symptoms in patients with head and neck cancer: an important relationship. Support Care Cancer. 2014;22(11):3053-60.
- Kam D, Salib A, Gorgy G, Patel TD, Carniol ET, Eloy JA, et al. Incidence of Suicide in Patients With Head and Neck Cancer. JAMA Otolaryngol Head Neck Surg. 2015;141(12):1075-81.
- Mehanna HM, De Boer MF, Morton RP. The association of psycho-social factors and survival in head and neck cancer. Clin Otolaryngol. 2008;33(2):83-9.
- Osthus AA, Aarstad AK, Olofsson J, Aarstad HJ. Health-related quality of life scores in long-term head and neck cancer survivors predict subsequent survival: a prospective cohort study. Clin Otolaryngol. 2011;36(4):361-8.
- Neilson K, Pollard A, Boonzaier A, Corry J, Castle D, Smith D, et al. A longitudinal study of distress (depression and anxiety) up to 18 months after radiotherapy for head and neck cancer. Psychooncology. 2013;22(8):1843-8.